Urea a Comprehensive Review of the Clinical Literature
Abstract
Urea is a hygroscopic molecule (capable of absorbing water) present in the epidermis as a component of the natural moisturizing factor (NMF) and is essential for the adequate hydration and integrity of the stratum corneum. Urea improves skin bulwark role including antimicrobial defence by regulating cistron expression in keratinocytes relevant for their differentiation and antimicrobial peptide production. It also plays a key role in regulating keratinocyte proliferation. One of the first uses of urea in mod medicine was the topical treatment of wounds due to its proteolytic and antibacterial properties. Now, urea is widely used in dermatology to improve skin barrier part and as one of the most common moisturizers and keratolytic agents. Urea-containing formulations are available in diverse formulations and concentrations. Multiple clinical trials on the use of urea-containing formulations have shown meaning clinical improvement in many of the dermatosis presenting with scaly and dry peel such as atopic dermatitis, ichthyosis, xerosis, seborrheic dermatitis and psoriasis, among others. Furthermore, urea can increase skin penetration and optimize the action of topical drugs. Urea-based products are well tolerated; their side effects are mild and are more frequent at high concentration. Here, we present a review of the use of urea in dermatology, discussing its machinery of action, safety profile and frequent indications.
FormalPara Central Summary Points
| Urea is widely used in dermatology to improve skin barrier function and as one of the virtually common moisturizers and keratolytic agents |
| Urea plays a fundamental office in regulating keratinocyte proliferation, the pare's barrier function and antimicrobial defense |
| Urea induces the expression of filaggrin, loricrin and transglutaminase-i, i.due east., genes which are important for keratinocyte differentiation and thus pare barrier function |
| Urea-containing formulations have shown significant clinical improvement in many of the dermatoses presenting with scaly and dry skin such equally atopic dermatitis, ichthyosis, xerosis, seborrheic dermatitis and psoriasis |
| It tin can be easily incorporated into dermatological preparations considering it is highly h2o soluble |
| Urea tin can increase skin and nail penetration and optimize the action of topical drugs |
| Compounds with depression urea concentration (2%–10%) are indicated for moisturizing and optimizing the skin's barrier office, medium concentration (10%–30%) for moisturizers and keratolytics and loftier concentrations (≥ xxx%) for keratolytics and debriding necrotic tissue |
Introduction
Urea is a depression-molecular-weight organic molecule composed of a carbonyl grouping fastened to two amine residues. It is produced mainly afterwards hepatic digestion of proteins. Urea is a hygroscopic molecule (capable of absorbing water) present in the epidermis every bit a component of the natural moisturizing gene (NMF) and is essential for the adequate hydration and integrity of the stratum corneum. A reduction in the hygroscopic capacity of the peel tin can increase transepidermal water loss (TEWL), deregulate epidermal proliferation and inhibit pare desquamation, inducing hyperkeratosis and pruritus [1].
Urea is a topical emollient and moisturizing, keratolytic and antipruritic amanuensis, and it plays a central function in keratinocyte gene regulation. In Asia, Africa and Europe, the therapeutic use of urine (urotherapy) has been documented for centuries. Ane of the first uses of urea in modern medicine was the topical treatment of wounds due to its proteolytic and antibacterial properties [2]. Currently, urea is widely used in dermatology. It is prescribed for the treatment of various dermatoses presenting with scaly and dry out skin such as atopic dermatitis, ichthyosis, seborrheic dermatitis and psoriasis, among others [iii]. Furthermore, urea can increase pare penetration and optimize the action of topical drugs [3]. Urea-containing formulations are bachelor in diverse formulations and concentrations.
Topical urea is a well-tolerated treatment; its side furnishings are balmy and are more than frequent at high concentration. Here, we present a review of topical urea in dermatology, discussing its mechanism of action, safe profile, formulations and frequent indications.
This article is based on previously conducted studies and does non comprise any new studies with human participants or animals performed by any of the authors.
Safety Contour
Urea-based formulations are well tolerated. Urea-containing creams may present an unpleasant odor, acquired by volatile amine, only it dissipates rapidly [four]. Mild skin irritation is occasionally observed and can exist more frequent with use at higher concentration. This adverse effect is temporary and commonly self-resolving. We have only found 1 reported example of allergic contact dermatitis to a foam containing a high concentration of urea, among other components, and the agin effect was probably secondary to an ingredient other than urea [5].
Machinery of Activeness
- 1.
Increases moisturization of the stratum corneum (Table 1).
Urea reduces TEWL and increases h2o retention and the resistance of the stratum corneum against osmotic stress. Furthermore, urea can human action as an endogenous humectant replacing h2o in depression humidity conditions [6, 7].
- 2.
Improves skin'south barrier function and antimicrobial defence (Fig. 1):
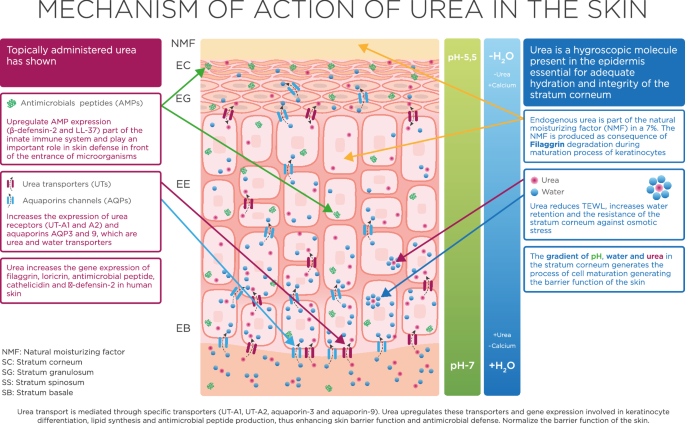
Mechanism of action of urea on the skin. Urea ship is mediated through specific transporters (UT-A1, UT-A2, aquaporin-3 and aquaporin-9). Urea upregulates these transporters and factor expression involved in keratinocyte differentiation, lipid synthesis and antimicrobial peptide production, thus enhancing skin barrier role and antimicrobial defense
Keratinocytes limited functionally active urea transporters. In this jail cell type, urea uptake was found to be associated with active regulation of the transcriptional expression of genes encoding for urea transporters and beyond. Specifically, urea induces the expression of filaggrin, loricrin and transglutaminase-1, i.e., genes which are important for keratinocyte differentiation and thus skin barrier function [8]. Transglutaminase-1 catalyzes the formation of isopeptide protein–protein crosslinks, allowing the construction of the mechanically resistant envelope composed of proteins such as involucrin and locrinin (its major component), which encloses corneocytes [8]. Filaggrin is a crucial epidermal protein which contributes to the structure of the stratum corneum and to pare barrier function. Filaggrin mutations can exist observed in genodermatoses such as ichthyosis vulgaris, caused by loss-of-function mutations in the filaggrin gene, and characterized by dry skin and scaling, or in inflammatory chronic dermatoses such every bit atopic dermatitis (AD) [half dozen]. AD patients with filaggrin mutations take more frequent hospital admissions and reduced wellness-related quality of life than Ad individuals with wild-blazon fillagrin [6]. Filaggrin expression has shown the strongest upregulation after urea treatment [8]. This is in line with the observation that urea treatment was found to normalize skin barrier function and to upregulate AMP expression in a murine model of Advert [viii]. Accordingly, controlled clinical studies accept demonstrated that topical application of urea is effective in reducing TEWL and thus in improving skin bulwark office. Urea also induces the transcriptional expression of the antimicrobial peptides cathelicidin and β-defensin-ii in cultured keratinocytes in vitro and in human skin in vivo, further emphasizing its effectiveness in improving pare bulwark role [8].
- 3.
Regulates epidermal proliferation
Urea is a highly active molecule and an important regulator of epidermal structure and part. Urea plays a fundamental role in controlling keratinocyte proliferation: information technology decreases Deoxyribonucleic acid synthesis in basal cells and prolongs the generation time of post-mitosis epidermal cells. Urea induces a reduction in cellularity, resulting in epidermal thinning [9].
- 4.
Keratolytic activity
Urea at higher concentrations can denature proteins such as keratin by breaking their hydrogen bonds [6] or by inducing conformational changes in their poly peptide structure [3].
- 5.
Increases drug penetration
Urea can facilitate the transport of molecules such as antifungals, corticosteroids and hormones through the peel and nails. This issue seems to be secondary to increased h2o assimilation by keratinocytes in the presence of urea and to its keratolytic action [6].
Topical Formulations Containing Urea
Urea can exist easily incorporated into dermatological preparations because it is highly h2o soluble. There are multiple vehicles and formulations (creams, lotions, emulsions, ointments, gels, shampoos and nail lacquers, amid others) and concentrations of urea available in over-the-counter products and prescription medications, which allows great versatility in its prescription. Various factors must be considered before choosing the most adequate product: the disorder to be treated, severity, surface area of the body involved (and its extension) and corrective acceptability [10]. In general, compounds with depression urea concentration (2%–10%) are indicated for moisturizing and optimizing the skin's barrier function [eleven], medium concentration (10%–30%) for moisturizers and keratolytics [12] and high concentrations (≥ xxx%) for keratolytics and for debriding necrotic tissue [4] (Table 2).
Main Indications for Urea in Dermatology
Maintaining Salubrious Skin
Products with low or medium concentration (2%–xx%) of urea may be indicated for routine skin care in individuals without skin disorders [3, 3,xi,12,thirteen]. Urea can decrease TEWL [13], increase the water content of the stratum corneum, optimize the skin barrier role and upregulate antimicrobial peptides in the skin [8]. It has too been shown to decrease skin reactivity to irritants such every bit sodium lauryl sulfate [13]. Furthermore, the improver of 5% urea to a hydroalcoholic gel reduced TEWL, dryness and pare reactivity [fourteen]. Regulatory properties of urea at the epidermis could even assist to reduce pare aging [15].
Choosing an emollient/moisturizer among the vast diverseness of available products can be challenging. The platonic emollient/moisturizer should reduce TEWL, restore the skin barrier function, exist hypoallergenic, non-comedogenic and fragrance-free, exist easily absorbed and accept an adequate cost [x]. Urea-containing formulations can potentially offering these characteristics and exist indicated for maintaining good for you skin and for treating a wide range of skin disorders, equally discussed in the post-obit sections.
Atopic Dermatitis
The peel of patients with AD is characterized by increased TEWL and dysfunction of the skin barrier [16]. The use of emollient and moisturizing creams is considered a cornerstone of the management of this disorder [16, 17]. The touch on of moisturizers on Advert management has been documented in a large number of clinical trials of varying quality and blueprint [eighteen]. However, given the wide diversity of products available, choosing an emollient/moisturizer tin be difficult, and some products may fifty-fifty worsen AD or induce contact dermatitis [16, 18].
Urea-containing preparations have been shown to decrease TEWL and ameliorate hydration of the stratum corneum and water-binding capacity in eczematous skin [3, 11, 13, 19]. In a murine model of Ad, a urea-based formulation improved the antimicrobial defense and the barrier function of the skin by regulating genes involved in the production of antimicrobial peptides, differentiation of keratinocytes and lipid synthesis [8]. The use of topical urea at concentrations ranging from four% to 20% has been documented in multiple clinical trials [18,nineteen,20,21,22,23,24,25]. A systematic review of the utilize of emollients in AD found that clinical effectiveness appears most well documented for urea-based preparations and recommends topical urea as a first-line choice in Advertizing [18]. A randomized clinical trial (RCT) demonstrated the superiority of urea 4% versus glycerin twenty% in reducing TEWL in patients with AD [nineteen]. An RCT comparison 2 urea-based formulations (five% urea moisturizer vs 10% urea balm) found no significant differences between them in reducing the Scoring Atopic Dermatitis (SCORAD) severity index [22].
Regarding prevention of Advertizing relapse, an RCT including 172 Advertising patients showed that prolonged use of a grooming containing 5% urea significantly increased the eczema-costless fourth dimension, reducing the risk of relapse past 37% [21]. Similar findings were reported in another RCT on 53 individuals with hand eczema [xx].
Xerosis
Multiple clinical studies support the apply of urea-containing formulations at varying concentrations (virtually oft 10%) for the treatment of xerosis in individuals with or without skin disorders [3, 6]. A controlled clinical written report of 12 patients presenting with severe dry peel on the junior extremities showed a significant reduction in TEWL after twice-daily application of a 15% urea foam [26]. A placebo-controlled, double-blind report of 21 healthy individuals showed that a in one case-daily application of a 20% urea-containing foam led to a significant reduction of TEWL [8]. An experimental report of five healthy subjects has demonstrated that a 20% urea-based cream significantly increased the water content of the stratum corneum [27].
Xerosis in the elderly: Xerosis can touch up to 75% of older adults. In a prospective study of 42 individuals > threescore years old, application of a 5% urea-containing foam showed increased skin hydration compared to a control emollient [28]. In an experimental study of 10 patients with senile xerosis, the application of a 10% urea-based cream led to marked clinical improvement [29].
Xerosis in patients with diabetes mellitus: Xerosis is often observed in diabetic patients and tin increase the adventure of skin infection and ulceration. In an RCT of 40 individuals with type 2 diabetes mellitus, a five% urea-based formulation with other ingredients such as arginine and carnosine increased skin hydration and significantly decreased xerosis compared to a glycerol-based emollient [30]. In another RCT of 40 patients with diabetes > 60 years a moisturizer containing 10% urea provided faster and better clinical improvement of xerosis of the anxiety than a command emollient [31]. A double-blind pilot study of thirty diabetic individuals compared the efficacy of a cream containing ten% urea and a cream containing 25% urea in the treatment of anhydrosis in the diabetic foot. Although both urea creams induced a significant increase in pare hydration, the 25% urea cream produced ameliorate results [32].
Xerosis in hemodialyzed patients: Xerosis is very mutual amongst patients undergoing hemodialysis. Associated factors for the development of xerosis in these individuals include accumulation of uremic toxins, presence of comorbidities such as diabetes mellitus and viral hepatitis, and systemic inflammation, among others. An RCT on 15 hemodialysis patients with severe xerosis showed that the use of a lotion containing 10% urea and dexpanthenol led to significant clinical improvement and reduction in pruritus [33].
Foot xerosis: Xerosis of the feet is a very mutual condition. A systematic review of the literature revealed that emollients containing urea have been the most researched [34]. Fourteen studies using urea in varying concentration (five%–40%) have shown good clinical responses [34].
Ichthyosis
Ichthyoses are a grouping of genetic disorders characterized by cutaneous xerosis. Ichthyosis vulgaris (IV) is the near prevalent subtype. More than a dozen clinical trials carried out on patients with various ichthyoses, using urea-based formulations at concentrations ranging from 2% to 10% (x% has been the most ofttimes used), have shown significant improvement of clinical parameters together with increased water retentiveness chapters of the stratum corneum [3, eleven]. In an RCT on 30 4 patients, a 10% urea formulation demonstrated a greater reduction in flaking, roughness, redness and smashing compared to a glycerol-based emollient cream [35]. In a double-blind clinical trial on 84 IV individuals, a urea-based cream was significantly improve in decision-making the ichthyosis than ii% salicylic acid ointment and paraffin [36]. In a prospective study on five patients with IV, a ten% urea-containing emulsion significantly decreased pruritus and xerosis in all individuals. Videodermatoscopy and confocal reflectance microscopy were performed, revealing a marked reduction in desquamation and normalization of furrow size and morphology [37]. In patients with Iv, urea tin not only increment stratum corneum hydration, but may as well upregulate filaggrin cistron expression [11, 37].
Psoriasis
Urea-based formulations can improve hydration of the stratum corneum and its water retentivity capacity and decrease TEWL, pruritus, desquamation and hyperkeratosis in patients with psoriasis [3, 4, 12, 38]. High urea concentration (40%–l%) tin be an excellent alternative in the treatment of localized hyperkeratotic plaques of psoriasis [4]. Urea at 40% together with bifonazole 1% tin be effective in the management of scalp psoriasis [3]. Medium urea concentration (17%) together with 0.1% dithranol has shown good clinical responses [3]. In an RCT on lxx patients with scalp psoriasis, the utilise of a urea-based shampoo significantly reduced itching and psoriasis severity index scores [39]. While medium or loftier urea concentration is usually indicated in psoriasis, some studies support the use of low urea concentration (5% to 12%) [12]. Urea at low concentration can also increment the effectiveness of topical betamethasone and calcipotriol [xi, 38].
Hyperkeratosis and/or Palmoplantar Keratodermas
Palmoplantar keratodermas are a wide spectrum of acquired and hereditary disorders characterized past abnormal thickening of the skin on the palms and soles. Urea at > thirty% concentration may exist a skillful culling for symptomatic treatment [12, xl]. Urea tin can be indicated together with topical salicylic acrid, lactic acrid, retinoids and corticosteroids.
Targeted therapy has revolutionized cancer therapy, and a wide range of dermatologic adverse events has been described. Mitt-foot skin reaction (HFSR) is characterized by painful hyperkeratotic lesions on the palms and soles and can severely touch on health-related quality of life and lead to discontinuation or drug dose reduction. An RCT on 871 patients with advanced hepatocellular carcinoma treated with sorafenib showed that prophylactic treatment with a 10% urea-based cream can significantly reduce HFSR rates, extend the time to its first occurrence and ameliorate patient quality of life [41]. Similar findings were reported in a recent RCT on 288 patients under sorafenib therapy [42].
Irradiation-Induced Dermatitis
Radiation-induced dermatitis is one of the almost common side effects of radiations therapy. In a prospective report of 98 patients with breast cancer, intensive use of a balm containing iii% urea, polidocanol and hyaluronic acrid doubled the probability of not developing radiodermatitis during radiotherapy, and intensive use was more effective than standard use in reducing the incidence of skin toxicity and skin toxicity grade two or college [43].
Seborrheic Dermatitis of the Scalp
The almost ofttimes prescribed pharmacological treatments for seborrheic dermatitis are antifungals and corticosteroids. Urea has antifungal and antimicrobial properties together with high moisturizing capacity and a keratolytic effect. The apply of keratolytics can prevent scaling or crusting in patients with seborrheic dermatitis and can increase the penetration of topical drugs [44]. In a clinical written report of patients with mild-moderate seborrheic dermatitis, the use of a shampoo containing urea, glycolic acid, salicylic acid, pale ichthyol and laureth significantly reduced irritation and itching and improved hair appearance [forty]. The employ of a formulation containing 40% urea and 1% bifonazole may exist an option in severe cases [3].
Actinic Keratosis and Cancerization Field
Treatment of hyperkeratotic actinic keratoses tin be challenging. Pretreatment with keratolytics such as urea-based formulations at high concentration (40%), salicylic acid or topical retinoids can increase response rates [45].
Nail Disorders
Urea at forty%–fifty% has been extensively used for the treatment of blast disorders; information technology can enhance nail permeability and soften the nail plate [4]. Urea at medium or high concentrations can improve the efficacy of topical antifungal drugs by increasing penetration and biodisponibility [iv, vi, 12]. A recent systematic review showed that forty% urea plus topical antifungals tin can induce clinical comeback in 29%–85% of cases [46].
Urea at loftier concentration can be an first-class culling in the management of smash psoriasis, onychogryphosis and pincer nails, amongst others, equally it can allow cut and proper care of thickened nails, reducing patient discomfort, with minimal associated adverse events. The application of urea nether occlusion leads to faster clinical responses [4].
Tinea Pedis
Tinea pedis can accept a chronic and recalcitrant course. Urea has antimicrobial backdrop and reduces flaking and cracks. The apply of urea at low concentration (10%) together with topical antifungals can reduce treatment duration and better clinical response [ii]. Urea at high concentration tin can be useful in the management of hyperkeratotic tinea pedis.
Conclusions
Urea plays a fundamental office in regulating keratinocyte proliferation, the skin'southward barrier part and antimicrobial defense. Urea-based formulations are well tolerated and one of the most commonly prescribed moisturizers and keratolytic agents for dermatologic patients. Urea-containing formulations tin be indicated to maintain healthy peel and treat a broad range of peel disorders such every bit Ad, xerosis, psoriasis, ichthyosis and seborrheic dermatitis, among many others, and to meliorate penetration of topical drugs into the skin and nails.
The furnishings of urea on gene expression predict, in the near future, a relevant role for urea-containing formulations for skin barrier therapy.
References
-
Friedman AJ, von Grote EC, Meckfessel MH. Urea: a clinically oriented overview from demote to bedside. J Drugs Dermatol. 2016;xv:633–nine.
-
Verzì AE, Musumeci ML, Lacarrubba F, Micali G. History of urea as a dermatological agent in clinical practise. Int J Clin Pract. 2020;74(Suppl 187):e13621.
-
Pan M, Heinecke G, Bernardo S, et al. Urea: a comprehensive review of the clinical literature. Dermatol Online J. 2013;19:20392.
-
Starace K, Alessandrini A, Piraccini BM. Clinical evidences of urea at high concentration on skin and annexes. Int J Clin Pract. 2020;74(Suppl 187):e13740.
-
Piraccini BM, Alessandrini A, Bruni F, Starace M. Astute periungueal dermatitis induced by awarding of urea-containing cream nether occlusion. J Dermatol Example Rep. 2012;half-dozen:xviii–twenty.
-
Celleno L. Topical urea in skincare: a review. Dermatol Ther. 2018;31:12690.
-
Trullàs-Cabanes C, Mirada-Ferré A, Salomon-Niera K. El valor de la urea en el cuidado y tratamiento de la piel. Revista Dermatológica Perú. 2008;eighteen(1):41–4.
-
Grether-Brook S, Felsner I, Brenden H, et al. Urea uptake enhances bulwark office and antimicrobial defence force in humans by regulating epidermal factor expression. J Invest Dermatol. 2012;132:1561–72.
-
Berardesca E, Cameli N. Not-invasive assessment of urea efficacy: a review. Int J Clin Pract. 2020;74(Suppl 187):e13603.
-
Sethi A, Kaur T, Malhotra South, Gambhir M. Moisturizers: the slippery road. Indian J Dermatol. 2016;61:279–87.
-
Lacarrubba F, Nasca MR, Puglisi DF, Micali M. Clinical evidences of urea at low concentration. Int J Clin Pract. 2020;74(Suppl 187):e13626.
-
Dall'Oglio F, Tedeschi A, Verzì AE, et al. Clinical evidences of urea at medium concentration. Int J Clin Pract. 2020;74:e13815.
-
Loden M. Urea-containing moisturizers influence barrier properties of normal skin. Arch Dermatol Res. 1996;288:103–7.
-
Lodén Grand. Ethanol-based disinfectants containing urea may reduce lather sensitivity. Dermatitis. 2020;31:328–32.
-
Sanz MT, Campos C, Milani M, et al. Biorevitalizing effect of a novel facial serum containing apple tree stem prison cell extract, pro-collagen lipopeptide, creatine, and urea on pare crumbling signs. J Cosmet Dermatol. 2016;15:24–30.
-
Wollenberg A, Christen-Zäch S, Taieb A, et al. ETFAD/EADV Eczema task forcefulness 2020 position paper on diagnosis and treatment of atopic dermatitis in adults and children. J Eur Acad Dermatol Venereol. 2020;34:2717–44.
-
Garnacho-Saucedo G, Salido-Vallejo R, Moreno-Giménez JC. Atopic dermatitis: update and proposed management algorithm. Actas Dermosifiliogr. 2013;104:4–sixteen.
-
Lindh JD, Bradley M. Clinical effectiveness of moisturizers in atopic dermatitis and related disorders: a systematic review. Am J Clin Dermatol. 2015;sixteen:341–59.
-
Lodén Thou, Andersson Air-conditioning, Andersson C, et al. Instrumental and dermatologist evaluation of the outcome of glycerine and urea on dry skin in atopic dermatitis. Peel Res Technol. 2001;vii:209–13.
-
Lodén Thou, Wirén K, Smerud 1000, et al. Handling with a barrier-strengthening moisturizer prevents relapse of hand-eczema. An open up, randomized, prospective, parallel grouping study. Acta Derm Venereol. 2010;90:602–six.
-
Åkerström U, Reitamo S, Langeland T, et al. Comparing of moisturizing creams for the prevention of atopic dermatitis relapse: a randomized double-blind controlled multicentre clinical trial. Acta Derm Venereol. 2015;95:587–92.
-
Bissonnette R, Maari C, Provost North, et al. A double-blind study of tolerance and efficacy of a new urea-containing moisturizer in patients with atopic dermatitis. J Cosmet Dermatol. 2010;9:16–21.
-
Lodén M, Andersson A-C, Anderson C, et al. A double-bullheaded study comparing the outcome of glycerin and urea on dry, eczematous peel in atopic patients. Acta Derm Venereol. 2002;82:45–7.
-
Hagströmer L, Nyrén M, Emtestam L. Do urea and sodium chloride together increase the efficacy of moisturisers for atopic dermatitis skin? A comparative, double-bullheaded and randomised study. Peel Pharmacol Appl Skin Physiol. 2001;14:27–33.
-
Nasrollahi SA, Ayatollahi A, Yazdanparast T, et al. Comparison of linoleic acrid-containing h2o-in-oil emulsion with urea-containing h2o-in-oil emulsion in the treatment of atopic dermatitis: a randomized clinical trial. Clin Cosmet Investig Dermatol. 2018;11:21–8.
-
Rosado C, Pinto P, Rodrigues LM. Cess of moisturizers and barrier function restoration using dynamic methods. Pare Res Technol. 2009;15:77–83.
-
Egawa M. In vivo simultaneous measurement of urea and water in the homo stratum corneum by diffuse-reflectance virtually-infrared spectroscopy. Skin Res Technol. 2009;15:195–nine.
-
Danby SG, Chocolate-brown Grand, Higgs-Bayliss T, et al. The event of an emollient containing urea, ceramide NP, and lactate on skin bulwark structure and function in older people with dry peel. Peel Pharmacol Physiol. 2016;29:135–47.
-
Horii I, Nakayama Y, Obata K, Tagami H. Stratum corneum hydration and amino acid content in xerotic peel. Br J Dermatol. 1989;121:587–92.
-
Federici A, Federici G, Milani Yard. An urea, arginine and carnosine based cream (Ureadin Rx Db ISDIN) shows greater efficacy in the handling of severe xerosis of the feet in Type 2 diabetic patients in comparison with glycerol-based emollient cream. A randomized, assessor-blinded, controlled trial. BMC Dermatol. 2012;12:16.
-
Pham HT, Exelbert 50, Segal-Owens AC, Veves A. A prospective, randomized, controlled double-blind study of a moisturizer for xerosis of the anxiety in patients with diabetes. Ostomy Wound Manage. 2002;48:30–6.
-
Baird SA, Skinner CM, Trail S, Frankis JS. Anhydrosis in the diabetic foot: a comparison of two urea creams. Diabetic Foot J. 2003;6:four.
-
Castello Thou, Milani Yard. Efficacy of topical hydrating and emollient lotion containing 10% urea ISDIN® plus dexpanthenol (Ureadin Rx 10) in the handling of pare xerosis and pruritus in hemodialyzed patients: an open up prospective airplane pilot trial. K Ital Dermatol Venereol. 2011;146:321–5.
-
Parker J, Scharfbillig R, Jones S. Moisturisers for the treatment of foot xerosis: a systematic review. J Foot Ankle Res. 2017;x:9.
-
Tadini Grand, Giustini S, Milani M. Efficacy of topical 10% urea-based lotion in patients with ichthyosis vulgaris: a two-eye, randomized, controlled, unmarried-blind, right-vs.-left study in comparison with standard glycerol-based emollient cream. Curr Med Res Opin. 2011;27:2279–84.
-
Pope FM, Rees JK, Wells RS, Lewis KG. Out-patient treatment of ichthyosis: a double-blind trial of ointments. Br J Dermatol. 1972;86:291–6.
-
Benintende C, Boscaglia S, Dinotta F, et al. Treatment of ichthyosis vulgaris with a urea-based emulsion: videodermatoscopy and confocal microscopy evaluation. G Ital Dermatol Venereol. 2017;152:555–nine.
-
Jacobi A, Mayer A, Augustin M. Keratolytics and emollients and their role in the therapy of psoriasis: a systematic review. Dermatol Ther (Heidelb). 2015;v:1–18.
-
Rossi A, Pranteda Thou, Iorio A, et al. Efficacy of Iralfaris shampoo in the treatment of scalp psoriasis: a videodermoscopy evaluation prospective study in seventy patients. G Ital Dermatol Venereol. 2012;147:625–30.
-
Piraccini BM, Brandi N, Alessandrini A, et al. Efficacious and safe management of thick scales, redness and flaky scalp condition using a specific shampoo containing urea, glycolic acid, salicylic acrid, icthyol pale and laureth 9. zilch. 2018;five:1475095.
-
Ren Z, Zhu K, Kang H, et al. Randomized controlled trial of the prophylactic effect of urea-based cream on sorafenib-associated hand-human foot skin reactions in patients with advanced hepatocellular carcinoma. J Clin Oncol. 2015;33:894–900.
-
Lee Y-Due south, Jung YK, Kim JH, et al. Effect of urea cream on sorafenib-associated hand-human foot pare reaction in patients with hepatocellular carcinoma: a multicenter, randomised, double-blind controlled study. Eur J Cancer. 2020;140:19–27.
-
Pardo Masferrer J, Murcia Mejía K, Vidal Fernández K, et al. Prophylaxis with a cream containing urea reduces the incidence and severity of radio-induced dermatitis. Clin Transl Oncol. 2010;12:43–8.
-
Piquero-Casals J, Hexsel D, Mir-Bonafé JF, Rozas-Muñoz E. Topical non-pharmacological treatment for facial seborrheic dermatitis. Dermatol Ther (Heidelb). 2019;nine:469–77.
-
Piquero-Casals J, Morgado-Carrasco D, Gilaberte Y, et al. Management pearls on the treatment of actinic keratoses and field cancerization. Dermatol Ther (Heidelb). 2020. https://doi.org/10.1007/s13555-020-00425-4.
-
Dars S, Banwell HA, Matricciani L. The use of urea for the treatment of onychomycosis: a systematic review. J Human foot Ankle Res. 2019;12:22.
Acknowledgements
Funding
The journal'southward Rapid Service Fee was supported by ISDIN.
Authorship
All named authors run into the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this commodity, take responsibility for the integrity of the work as a whole, and have given their approving for this version to be published.
Writer Contributions
Jaime Piquero-Casals, Daniel Morgado-Carrasco, Corinne Granger and Jean Krutmann contributed equally to concept and blueprint of the study. Jaime Piquero-Casals, Daniel Morgado-Carrasco, Corinne Granger, Carles Trullàs, América Jesús-Silva and Jean Krutmann contributed to the draft and revised the manuscript.
Disclosures
Jaime Piquero-Casals, Daniel Morgado-Carrasco, and Jean Krutmann have received consultant fees from ISDIN. Corinne Granger and Carles Trullàs are employees of ISDIN. América Jesús-Silva has nothing to disclose.
Compliance with Ethics Guidelines
This commodity is based on previously conducted studies and does not contain whatsoever studies with human participants or animals performed by any of the authors.
Data Availability
Data sharing is not applicable to this article equally no datasets were generated or analyzed during the current study.
Writer data
Affiliations
Corresponding author
Rights and permissions
Open Access This commodity is licensed nether a Creative Commons Attribution-NonCommercial iv.0 International License, which permits any non-commercial utilize, sharing, adaptation, distribution and reproduction in whatsoever medium or format, as long as yous give appropriate credit to the original author(south) and the source, provide a link to the Creative Commons licence, and betoken if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the cloth. If material is not included in the article's Creative Commons licence and your intended utilize is not permitted by statutory regulation or exceeds the permitted use, you will demand to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/past-nc/4.0/.
Reprints and Permissions
About this article
Cite this article
Piquero-Casals, J., Morgado-Carrasco, D., Granger, C. et al. Urea in Dermatology: A Review of its Emollient, Moisturizing, Keratolytic, Pare Bulwark Enhancing and Antimicrobial Properties. Dermatol Ther (Heidelb) xi, 1905–1915 (2021). https://doi.org/x.1007/s13555-021-00611-y
-
Received:
-
Published:
-
Event Appointment:
-
DOI : https://doi.org/x.1007/s13555-021-00611-y
Keywords
- Urea
- Keratinocytes
- Atopic dermatitis
- Ichthyosis
- Psoriasis
Source: https://link.springer.com/article/10.1007/s13555-021-00611-y
0 Response to "Urea a Comprehensive Review of the Clinical Literature"
Post a Comment